About CHD2-related disorders
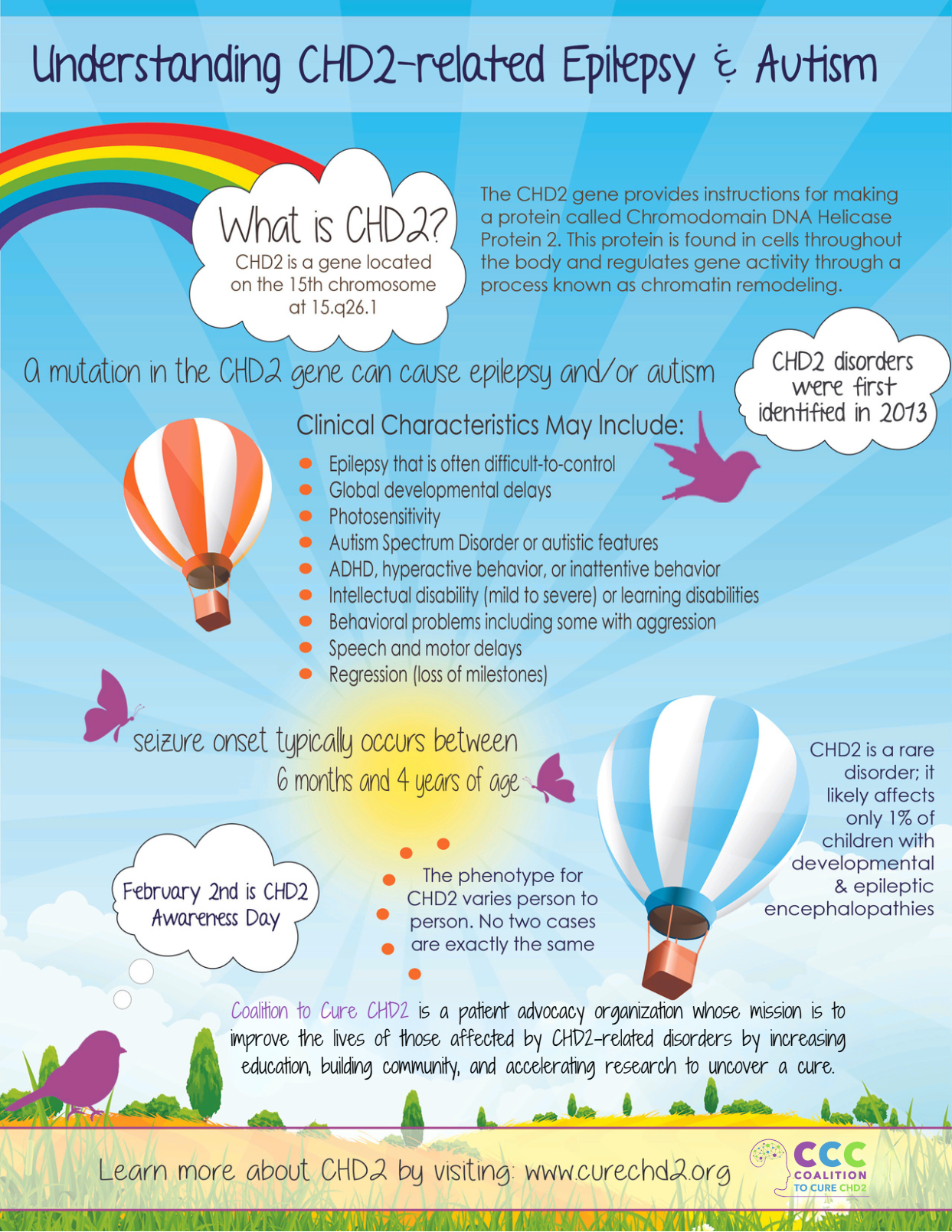
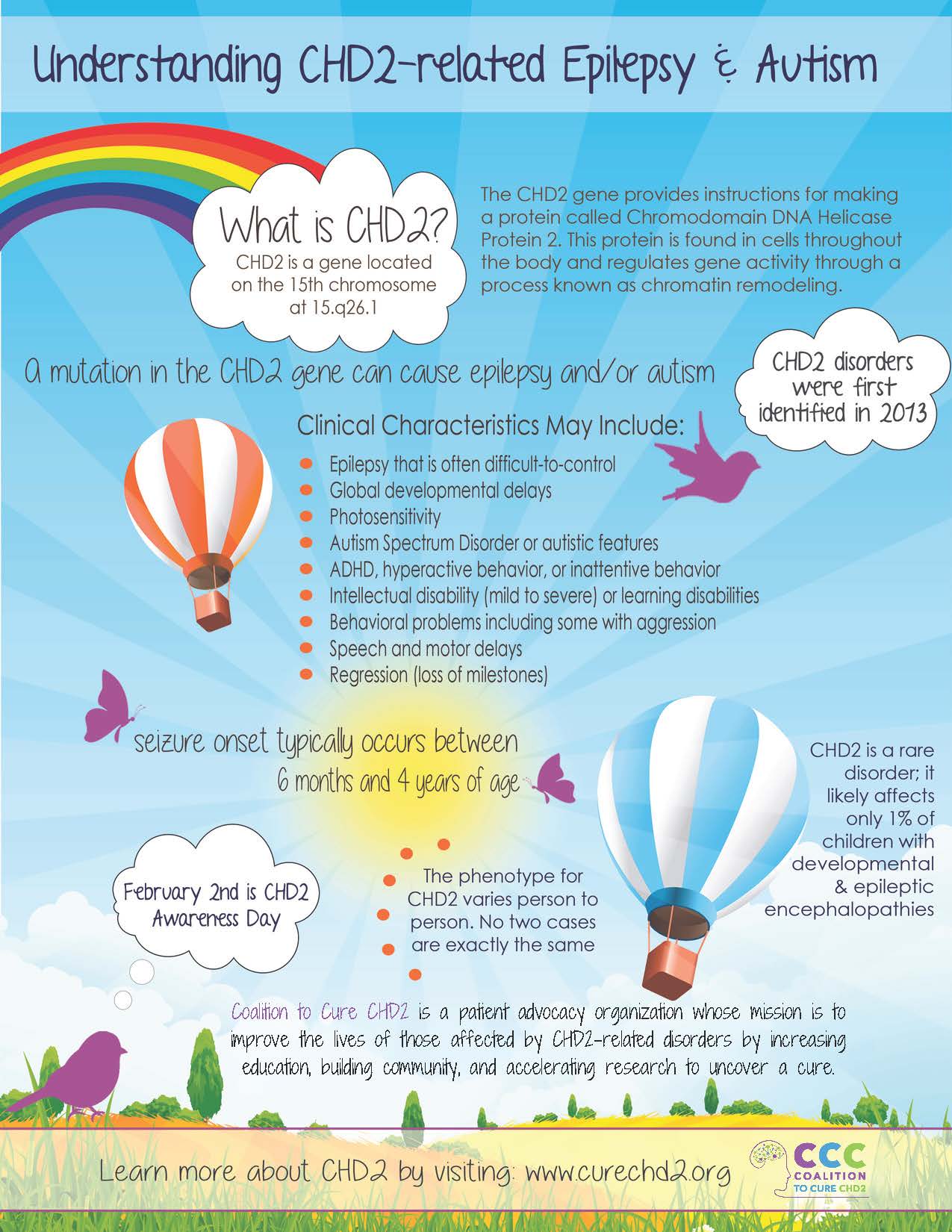
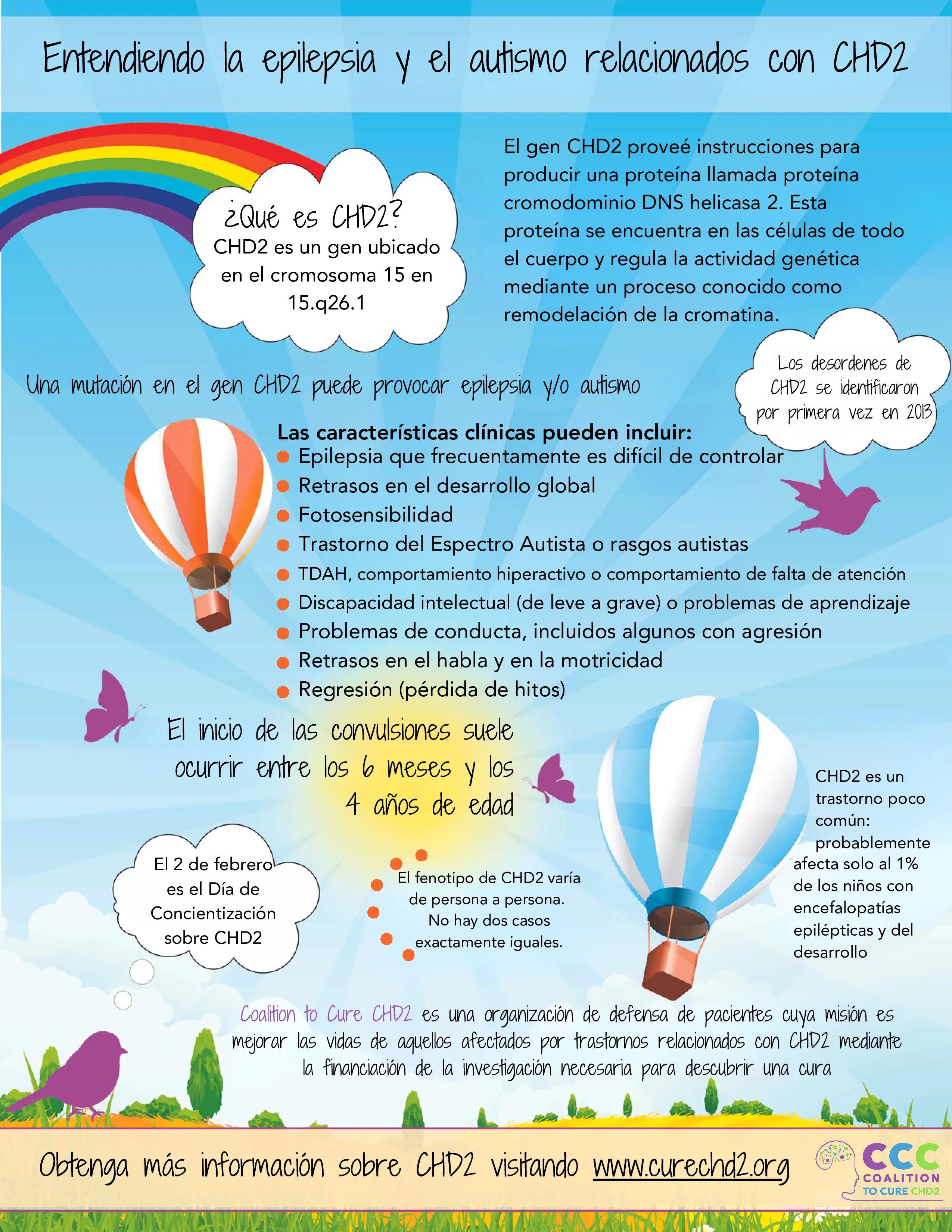
CHD2-related disorders are considered a developmental and epileptic encephalopathy (DEE), a group of disorders that are characterized by refractory or drug-resistant epilepsy, developmental delays. Typically, CHD2-related disorders present between ages six months and four years. Although most individuals with CHD2-related disorders have seizures, there is a small subset (about 10%) of the population who do not have seizures.
Photosensitive epilepsy (seizures caused by flashing lights and from looking at certain patterns) is common in individuals with CHD2-related disorders. Other symptoms may include intellectual disability, autism spectrum disorder, attention deficit hyperactivity disorder (ADHD), gastrointestinal problems (e.g., constipation), low muscle tone, and kyphoscoliosis (curvature of the spine).
Patients may experience developmental stagnation or regression – for example, a child may appear to be developing normally but then their speech or social skills stop improving or they may lose skills they had previously gained. Seizures have been seen to worsen at puberty; seizures may not improve in adulthood. Epilepsy syndromes that have common features to epilepsy in patients with CHD2 genetic variants include: Lennox-Gastaut Syndrome, Jeavons Syndrome (eyelid myoclonia with absence), Doose Syndrome (epilepsy with myoclonic atonic seizures) and West Syndrome (infantile epileptic spasms syndrome).
We continue to learn about ways CHD2 affects individuals. At this time, CHD2-related disorders are managed with treatments currently available such as anti-seizure medication; behavioral therapy; learning support; and occupational, physical, speech and language therapy, etc.
Read about the CHD2 Disease Concept Model here.
There is no targeted or specific genetic treatment for CHD2-related disorders, yet.
About the CHD2 Gene
CHD2 is a gene located on chromosome 15 that provides instructions for making a protein called chromodomain helicase DNA binding protein 2 (CHD2). This protein controls gene activity through a process called chromatin remodeling and therefore may play an important role in the brain, although its exact function is not well understood.
Changes in the CHD2 gene are usually not inherited; in most cases, the change only occurs in the affected person (de novo) and not their parents. However, the genetic change is autosomal dominant; therefore the affected person has a 50% chance of passing down this change to their offspring. The number of people affected by CHD2 is unknown but it is thought to be underdiagnosed. You can visit our map to see how many CHD2 families have been identified by Coalition to Cure CHD2.
There are no treatments or therapies specific to the CHD2 genetic disorder, but because a majority of individuals diagnosed with a CHD2 disorder have been diagnosed with autism spectrum disorders, intellectual disabilities and/or speech delays, therapies commonly used to treat these clinical features are commonly used to treat individuals with CHD2. These therapies include, but are not limited to, speech therapy, occupational therapy, physical therapy, behavioral therapy and psychological and developmental therapy. Specialists commonly seen include neurologists, orthopedists, dieticians, special needs dentists, gastroenterologists, geneticists and chiropractors.
A number of researchers and pharmaceutical companies are either currently working on, or are considering working on or investing in, the development of drugs or precision therapies that may improve the lives of those living with CHD2, or that may even lead to a cure for this disorder.
Coalition to Cure CHD2 was organized in 2020, which has the mission to improve the lives of those affected by CHD2-related disorders by increasing education, building community, and accelerating research to uncover a cure.
CHD2 Neurodevelopmental Disorders


Reviewed by: Dr. Charuta Joshi, pediatric neurologist, University of Texas Southwest Medical Center-Dallas Children's Hospital
Read about the CHD2 Disease Concept Model here.